NEONATAL DEATH IN PUBLIC MATERNITY OF REFERENCE: ASSOCIATED FACTORS
DOI:
https://doi.org/10.9789/2175-5361.rpcfo.v14.11264Keywords:
Newborn; Infant Mortality; Intensive Care Units; Risk factorsAbstract
Objective: To investigate maternal and neonatal factors associated with neonatal deaths in a reference maternity hospital in southwestern Maranhão. Methodology: Retrospective observational, quantitative study, with documental analysis in medical records. Brazil. Medical records of 677 neonates born in their own hospital in 2016 were selected. Results: Of the 677 medical records of admitted newborns, there were 14.2% of deaths and 85.8% of discharges, prematurity was the diagnosis among 42.4%, followed by 41.9% of respiratory disorders. The adjusted analysis of the model showed that neonatal death was associated with height <35cm (OR: 38.40; p<0.001) and 35-39cm (OR: 6.65, p<0.002), head circumference <22 cm (OR: 38.58; p<0.002) and Apgar in the 5th. minute <3 (OR: 5.91; p<0.001). Results: Of the 677 medical records of newborns admitted, there were 96 deaths (14.2%) and 581 discharges (85.8%), with prematurity being the most frequent diagnosis 287 (42.4%), followed by respiratory disorders 284 (41 , 9%). The adjusted analysis of the model showed that neonatal death was associated with height <35cm (OR: 38.40; p <0.001), height of 35-39cm (OR: 6.65, p <0.002), head circumference <22 cm (OR: 38.58; p <0.002) and Apgar in the 5th. minute <3 (OR: 5.91; p <0.001). Conclusions: Conclusion: Prematurity and respiratory disorders were the main causes of hospitalization. There is a need to review access to health services, as well as the implementation of qualified interventions in prenatal care, childbirth and birth.
Downloads
References
Morgan MC, Spindler H, Nambuya H, Nalwa GM, Namazzi G, Waiswa P, Otieno P, et al. Clinical cascades as a novel way to assess physical readiness of facilities for the care of small and sick neonates in Kenya and Uganda. PLoS One. [Internet]. 2018 [cited 2019 mai 5]; 13(11):e0207156. Available from: doi: 10.1371/journal.pone.0207156.
Farah AE, Abbas AH, Ahmed AT. Trends of admission and predictors of neonatal mortality: A hospital based retrospective cohort study in Somali region of Ethiopia. PLoS One. [Internet]. 2018 [cited 2019 mai 05];13: e0203314. Available from: doi:10.1371/journal.pone.0203314.
World Health Organization. Neonatal mortality rate. In: World Health Organization
[Internet]. 2018. [cited 2019 mai 06]. Available from: http://apps.who.int/gho/data/node.sdg.3-2-viz-3?lang=en
Varela AR, Schneider BC, Bubach S, Silveira MF, Bertoldi AD, Duarte LSM, et al. Fetal, neonatal, and post-neonatal mortality in the 2015 Pelotas (Brazil) birth cohort and associated factors. Cad. Saude Publica. [Internet]. 2019 [cited 2020 fev 10]; 35(7):e00072918. Available from: doi:10.1590/0102-311x00072918
Mengesha HG, Wuneh AD, Lerebo WT, Tekle TH. Survival of neonates and predictors of their mortality in Tigray region, Northern Ethiopia: prospective cohort study. BMC Pregnancy Childbirth. [Internet]. 2016 [cited 2019 jun 18];16(1): 202. Available from: doi:10.1186/s12884-016-0994-9
Gaiva MAM, Fujimori E, Sato APS. Maternal and child risk factors associated with
neonatal mortality. Texto context enferm. [Internet]. 2016 [cited 2019 mai 05]; 25(4):1–9. Available from: doi:10.1590/010407072016002290015
Migoto MT, Oliveira RP de, Silva AMR, Freire MH de S. Early neonatal mortality and risk factors: a case-control study in Paraná State. Rev. Bras. Enferm. [Internet]. 2018 [cited 2019 abr 18];71: 2527–2534. Available from: doi:10.1590/0034-7167-2016-0586
Li Y, Quigley MA, Dattani N, Gray R, Jayaweera H, Kurinczuk JJ, et al. The contribution of gestational age, area deprivation and mother’s country of birth to ethnic variations in infant mortality in England and Wales: A national cohort study using routinely collected data. Simeoni U, editor. PLoS One. [Internet]. 2018 [cited 2019 abr 18]; 13(4):e0195146. Available from: doi:10.1371/journal.pone.0195146
Piening BC, Geffers C, Gastmeier P, Schwab F. Pathogen-specific mortality in very low birth weight infants with primary bloodstream infection. PLoS One. [Internet]. 2017 [cited 2019 mai 08]; 12(6):e0180134. Available from: doi:10.1371/journal.pone.0180134
Persson M, Razaz N, Tedroff K, Joseph KS, Cnattingius S. Five and 10 minute Apgar scores and risks of cerebral palsy and epilepsy: population based cohort study in Sweden. BMJ. [Internet]. 2018 [cited 2019 mai 18]; 360 k207. Available from: doi:10.1136/bmj.k207
Lima SS de, Silva SM da, Avila PES, Nicolau MV, Neves PFM das. Aspectos clínicos de recém-nascidos admitidos em Unidade de Terapia Intensiva de hospital de referência da Região Norte do Brasil. ABCS Heal Sci. [Internet]. 2015 [acesso em 20 de agosto 2019]; 40(2):62–68. Disponível em: doi:10.7322/abcshs.v40i2.732
Xavier Ferreira Vianna RC, De Souza Freire MH, Carvalho DR, Migotto MT. Perfil da mortalidade infantil nas Macrorregionais de Saúde de um estado do Sul do Brasil, no triênio 2012–2014. Espaço para a Saúde - Rev Saúde Pública do Paraná. [Internet]. 2016 [acesso em 20 de agosto 2019]; 17(2):32-40. Disponível em: doi:10.22421/1517-7130.2016v17n2p32
Malta DC, Duarte EC, Escalante JJC, Almeida MF de, Sardinha LMV, Macário EM, et al. Mortes evitáveis em menores de um ano, Brasil, 1997 a 2006: contribuições para a avaliação de desempenho do Sistema Único de Saúde. Cad Saude Publica. [Internet]. 2010 [acesso em 20 de agosto 2019]; 26(3):481–491. Disponível em: doi:10.1590/S0102-311X2010000300006
Medeiros RS. Insuficiência de leitos de UTI: crise do capital e mercantilização da saúde. Argum. [Internet]. 2018 [acesso em 20 de agosto 2019]; 10(1):229-240. Disponível em: doi: http://10.18315/argumentum.v10i1.18647
Brasil (MS). Mortalidade no Brasil. In: DATASUS, Departamento de Informática do
Sistema Único de Saúde (TABNET) [Internet]. 2019 p. 1. [acesso em 20 de agosto 2019].Disponível em: http://tabnet.datasus.gov.br/cgi/deftohtm.exe?sim/cnv/obt10br.def
Coulibaly A, Baguiya A, Millogo T, Meda IB, Koueta F, Kouanda S. Predictors of
mortality of low birth weight newborns during the neonatal period: A cohort study in two health districts of Burkina Faso. Int J Gynecol Obstet. [Internet]. 2016 [cited 2019 jun 18]; 135:S89–S92. Available from: doi:10.1016/j.ijgo.2016.08.006
Ndombo PK, Ekei QM, Tochie JN, Temgoua MN, Angong FTE, Ntock FN, et al. A
cohort analysis of neonatal hospital mortality rate and predictors of neonatal mortality in a sub-urban hospital of Cameroon. Ital J Pediatr. [Internet]. 2017 [cited 2019 mai 08]; 43(1):52. Available from: doi:10.1186/s13052-017-0369-5
Chow S, Chow R, Popovic M, Lam M, Popovic M, Merrick J, et al. A Selected Review of the Mortality Rates of Neonatal Intensive Care Units. Front Public Heal. [Internet]. 2015 [cited 2019 mai 08]; 3:1-18. Available from: doi:10.3389/fpubh.2015.00225
Razeq NMA, Khader YS, Batieha AM. The incidence, risk factors, and mortality of preterm neonates: A prospective study from Jordan (2012-2013). Turkish J Obstet Gynecol. [Internet]. 2017 [cited 2019 mai 18]; 14: 28–36. Available from: doi:10.4274/tjod.62582
Osterman MJK, Kochanek KD, MacDorman MF, Strobino DM, Guyer B. Annual Summary of Vital Statistics: 2012-2013. Pediatrics. [Internet]. 2015 [cited 2019 mai 18]; 135(6):1115–1125. Available from: doi:10.1542/peds.2015-0434
França EB, Lansky S, Rego MAS, Malta DC, França JS, Teixeira R, et al. Principais causas da mortalidade na infância no Brasil, em 1990 e 2015: estimativas do estudo de carga global de doença. Rev Bras epidemiol. [Internet]. 2017 [acesso em 20 de agosto 2019]; 20 sUppl 1: 46-60. Disponível em: doi: 10.1590/1980-5497201700050005
Roussenq KR, Scalco JC, Rosa GJ da, Honório GJ da S, Schivinski CIS. Rebalancing thoracoabdominal movements in preterms infants: effects on cardiorespiratory parameters, in behavior, in pain and in the respiratory effort. Acta Fisiátrica. [Internet]. 2013 [cited 2019 jun 08]; 20(3):118–123. Available from: doi:10.5935/0104-7795.20130019
Tsai M, Lee I, Chu S, Lien R, Huang HR, Chiang MC, et al. Clinical and Molecular Characteristics of Neonatal Extended-Spectrum β-Lactamase-Producing Gram-Negative Bacteremia: A 12-Year Case-Control-Control Study of a Referral Center in Taiwan. PLoS One. [Internet]. 2016 [cited 2019 mai 18]; 11:e0159744. Available from: doi:10.1371/journal.pone.0159744
Rodrigues EC, Alves BCA, daVeiga GL, Adami F, Carlesso JS, Figueiredo FWS, et al. Neonatal mortality in Luanda, Angola: what can be done to reduce it? J Hum Growth. [Internet]. 2019 [cited 2019 mai 18]; 29(2):161-168. Available from: DOI: http://doi.org/10.7322/jhgd.v29.9415
Souza AMG, Souza TA, Ferreira TLS, Medeiros JSS, Souza DRS, Andrade FB.
Perfil epidemiológico da mortalidade neonatal no rio grande do norte-brasil: um estudo de base secundária. Revista Ciência Plural. [Internet]. 2018 [acesso em 20 de agosto 2019]; 4(2):115-127. Disponível em: https://periodicos.ufrn.br/rcp/article/view/16844/11271
Published
Versions
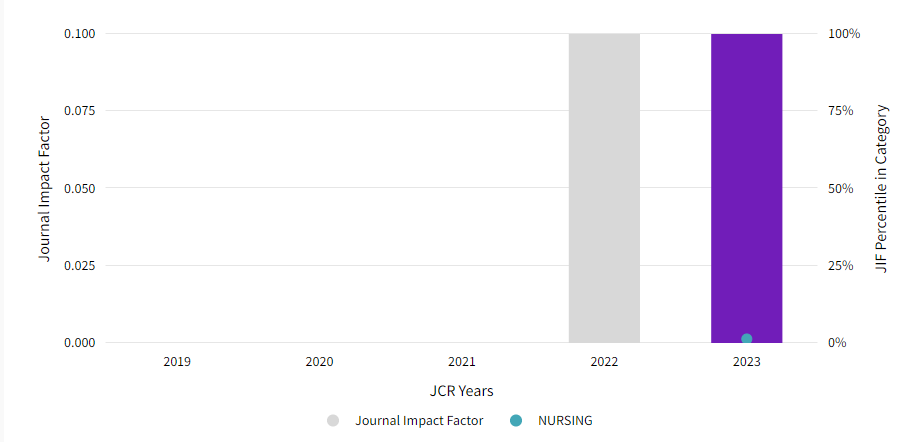
- 2022-08-15 (6)
- 2022-08-15 (5)
- 2022-08-12 (4)
- 2022-08-11 (3)
- 2022-08-11 (2)
- 2022-07-25 (1)
How to Cite
Issue
Section
License
Copyright (c) 2022 Revista de Pesquisa Cuidado é Fundamental Online

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
TRANSFER AGREEMENT COPYRIGHT I transfer copyright of the article to the Journal of Care Survey is Fundamental - Online - RPCF, so it is accepted due to electronic publishing. The copyright includes the right to reproduce in whole or in part by any means, distributing that article, including figures, photographs, and any translations. The author can also print and distribute copies of your article, stating that since the rights belong to RPCF. I declare that this manuscript is original and has not been submitted for publication, in whole or in part to other online journals or not, so BMMC in the Annals of scientific events or book chapters.